Also see part 2 - Pitfalls in DFA a1 - Polar belt position
Over the past several months, we have examined various factors that could affect DFA a1 values. Since this index depends upon fractal correlation patterns of cardiac beat intervals, precise measurement and proper algorithmic processing is essential. Therefore, excess artifact correction, sub optimal preprocessing (detrending of data) and poor R wave definition can all bias the DFA a1 value, resulting in erroneous intensity thresholds and exercise load management guidelines. The "low a1 while running" issue may yet represent another factor biasing the true measurement of this index. Along the path of seeking better DFA a1 accuracy, I have noted (and posted) that depending on ECG electrode placement, different DFA a1 can values occur. More recently, while looking at 12 lead ECG exercise ramp recordings (thanks to TG), I was astonished that depending on the lead selected to import into Kubios, quite different DFA a1 curves were produced. This post is an initial exploration into HRM belt placement and DFA a1. After reading through this material, you may want to consider a modified HRM placement for optimal a1 results and/or tinkering with position to prevent the "low a1 while running".
Background:
Depending on where on the body we measure the electrical activity of a cardiac cycle, different waveform shapes will be produced. Here is a rough guide on conventional ECG leads FYI.
There is also a concept called axis deviation - axis referring to the net electrical activity observed. If one chamber enlarges, the axis may change. It can also change with breathing
Lead placement and HRV
It has been shown that ECG lead placement does have an effect on both waveform signal and conventional HRV indexes. Let's review the study done (healthy subjects at rest in supine position). Although they did not perform standard 12 lead ECG's we still can get a sense of what is occurring.
Here is a representative comparison of the leads tested (lead 2 is the closest to standard HRM belts placed in the center of the chest).
We can see that the voltages and "sharpness" of the R peak are all very different.
The voltage comparison per lead:
 |
Although lead 2 did have a better R peak than most, there was tremendous variability in signal voltage (especially lead 3 which is in a location very "near" lead 2).
This was reflected in the differences between an averaged value (based on all leads) and each individual lead:
Finally their conclusion:
Although they conjectured about the respiratory change, it is well known that cardiac axis will shift with respiration. What is cardiac axis - as noted above, it's the net electrical direction of heart muscle electrical activity. Cardiac axis (and therefore waveform) will change during breathing and position
Although I did not recognize why at the time - my previous guess that my Movesense ECG waveform distortion was caused by diaphragm activity was somewhat partially correct. But it's not diaphragm muscle EMG distortion, it is actual cardiac axis shift when the HRM belt is in that particular location.Summary so far:
- ECG waveform alteration can change HRV at rest.
- Body position and respiration can alter cardiac axis - which in turn alters waveform.
Some examples:
First - a 12 lead ECG Ramp (sample rate 500 Hz) in an experienced triathlete: This was analyzed by Kubios and represents the same ramp/time sequence. We are looking at 3 leads - Lead 2, V3 and V5.
- There should no difference based on artifact, timing, since the signal measurement is simultaneous.
- However, lead V3 reads much lower than lead 2 and V5
How do the waveforms look?
Lead 2:
Lead V5
- On first scrutiny, they all look fairly good (symmetry, voltage) but clearly there is a difference in a1 decline.
- However, V3 is much wider than the others and this might be an issue in deciding where the R peak falls and/or could have more cardiac axis shift with respiration, which increases through the ramp.
Waveforms with a Movesense ECG belt
The following were obtained with the Suunto Movesense ECG unit (512 Hz) in 4 positions by simply rotating the HRM belt
Sensor placed by the Axilla:
 |
Sensor Mid-line
Sensor rotated Left (by nipple)
Sensor rotated Right
- Very different shapes, voltages and potential cardiac axis shifting.
- Right vs Axillary show opposite cardiac axis polarity
Can the phenomena of HRV bias occur with conventional HRMs like a Polar H10? To answer that question, I did a series of ramps wearing 3 HRMs (2 x H10 and a Movesense ECG).
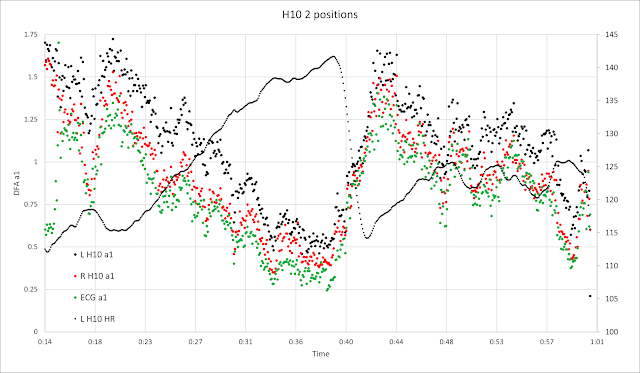
Ramp comparing L rotated H10 (R edge of sensor at midline) to R rotated H10 (L edge of sensor at midline) to rotated ECG (near axilla)
The results:
- Both the R rotated H10 and severely L rotated ECG are reading lower than the L rotated H10.
Ramp comparing H10 center vs H10 rotated L and ECG rotated L (similar to the H10).
- In this example all positions now show similar a1 values.
- It seems that R rotated or severely L rotated sensor positions may be affected by cardiac axis changes during respiration.
Example from another rider - Data obtained with Fatmaxxer, low artifact data. Session power, HR and sensor positions below, either Centered or rotated Left slightly.
Let's zoom in on the 2 identical intervals just after the mid portion:
- It appears that the left rotated positions displays higher a1 values than the center.
- This evidence is not as solid as simultaneously worn HRM or from a 12 lead ECG but is certainly suggestive.
- Higher a1 seen at moderate to high intensity usually implies that correlation patterns are still present. If one had the choice of the above sensor positions, it would be recommended to pick the Left position
To summarize:
- It has been shown that RR intervals and HRV can be subtlety different depending on the various leads in a resting ECG.
- This may be due due to alteration in waveform shape, voltage and cardiac axis shifts.
- These difference may be magnified during position change and especially respiration due to shifts in cardiac axis.
- During a 12 lead ECG recording of an athlete performing an exercise ramp, disparity in DFA a1 was seen in lead V3. This lead also had the widest R peak.
- It follows that HRM belt position could also be prone to variability in R peak precision depending on similar factors.
- For the majority of users, a center HRM position is probably fine. However, if one is seeing a lower DFA a1 on a regular basis than should be the case, a slight rotation of the HRM to the left may be something to try. This rotation could provide a more symmetrical waveform.
- Rotation of the HRM belt to the right is not recommended.
- Waveform voltage and shape can be inspected with Fatmaxxer and Excel, since it does capture ECG snippets.
- Runners affected by the low a1 issue (while running) could try alternate HRM belt placement to optimize shape, voltage and cardiac axis shifting.
- Interestingly, we did not see the low a1 phenomena with the participants in our validation study. However, the DFA a1 was derived from lead 2 ECG data, which happens to be an optimal lead.
- Finally - this observation should not reduce confidence in the ability of fractal correlation patterns to determine thresholds, fatigue and exercise loading. However, our conclusions are only as good as our data. Therefore optimization of HRM position should takes it's place along with artifact correction, HRM device quality/precision and data preprocessing as items to think about when using this methodology.
Heart rate variability during dynamic exercise
- Firstbeat VO2 estimation - valid or voodoo?
- Heart rate variability during exercise - threshold testing
- Exercise in the heat and VO2 max estimation
- DFA alpha1, HRV complexity and polarized training
- HRV artifact avoidance vs correction, getting it right the first time
- VT1 correlation to HRV indexes - revisited
- DFA a1 and Zone 1 limits - the effect of Kubios artifact correction
- HRV artifact effects on DFA a1 using alternate software
- A just published article on DFA a1 and Zone 1 demarcation
- DFA a1 vs intensity metrics via ramp vs constant power intervals
- DFA a1 decline with intensity, effect of elevated skin temperature
- Fractal Correlation Properties of Heart Rate Variability (DFA a1): A New Biomarker for Intensity Distribution in Endurance Exercise
- Movesense Medical ECG V2.0 Firmware brief review
- Movesense Medical ECG - improving the waveform and HRV accuracy
- DFA a1 and the aerobic threshold, video conference presentation
- DFA a1 - running ramp and sample rate observations with the Movesense ECG
- DFA a1 calculation - Kubios vs Python mini validation
- Frontiers in Physiology - Validation of DFA a1 as a marker of VT1
- Real time Aerobic thresholds and polarized training with HRV Logger
- Active Recovery with HRV Logger
- DFA a1 and exercise intensity FAQ
- DFA a1 agreement using Polar H10, ECG, HRV logger
- DFA a1 post HIT, and as marker of fatigue
- DFA a1 stability over longer exercise times
- DFA a1, Sample rates and Device quirks
- DFA a1 and the HRVT2 - VT2/LT2
- Low DFA a1 while running - a possible fix?
- Runalyze vs Kubios DFA a1 agreement
- DFA a1 - Runalyze vs Kubios vs Logger results in a cyclist
- Best practices for Runalyze and DFA a1 thresholds
- ACSM - HRVT validation in a cardiac disease population
- FatMaxxer - a new app for real time a1
- Another look at indoor exercise without a fan
- ECG artifact strips from Fatmaxxer - a guide
- ECG arrhythmia and artifact visualization tips
- DFA a1 as a marker of endurance exercise fatigue
- To train hard or not, that's the question
- DFA a1 HRVT and Ramp slope
- Pitfalls in DFA a1 - Polar belt position